We will learn in this article some common questions about women and heart disease. Heart disease is the leading cause of death for women in the United Kingdom. While about the same number of women and men die of the disease annually, fewer women survive their first heart attack. In many cases women don’t realize they are experiencing a heart attack since their symptoms aren’t always clear or well understood. Many times this results in the delay in getting treatment.
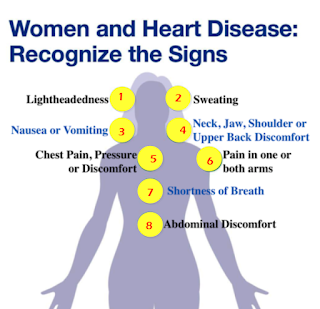
Women also have higher rates of additional medical problems, such as diabetes which contribute to worse outcomes. Women and men have similar symptoms of heart disease, including the most common symptoms of chest pain or shortness of breath; however women’s symptoms differ and they have a tendency to experience more of the less common symptoms. These may include throat tightness, left arm pain, or lightheadedness with activity.
Other less common symptoms include pain or discomfort in the upper back, arms, neck or jaw. Some people present only with a noticeable increase in fatigue or inability to do activities they once could do, especially in the elderly.
Yes, there are several. Polycystic ovarian syndrome is a condition that is often associated with obesity, hypertension and glucose intolerance, all traditional risk factors for heart disease. Some treatments for breast cancer may cause injury to the heart muscle. Turner syndrome is a genetic condition that affects only females, and they have a high incidence of hypertension and elevated cholesterol, as well as a greater likelihood of conditions that affect their an aorta.
Pregnancy-related conditions, such as premature birth, low birth weight, and pregnancy-induced hypertension, often are risk factors for heart disease later on. Postpartum cardiomyopathy, a condition in which the function of the heart reduces after giving birth and causes the heart to fail, is a life-threatening condition that can occur after delivery.
Just like in men, heart disease affects women of all ages; however, as we get older your heart disease risk increases. Menopause often brings with it an increase in cholesterol levels, hypertension, and weight gain which all can contribute to an increased risk of developing heart disease. The loss of protective estrogens also increases the risk of coronary heart disease in the post menopausal period.
We also commonly see women in the perimenopausal period presenting with palpitations due to hormonal changes. These can be quite disruptive to their lives. We divide risk into non-modifiable and modifiable categories. While age and family history are non-modifiable, there are modifiable risk factors that can reduce a woman’s overall risk.
These include maintaining a healthy weight, engaging in regular exercise at least 30 minutes most days of the week, eating a heart-healthy diet low in fat and high in fiber, fruits and vegetables, knowing your numbers by maintaining a healthy blood pressure less than 120 over 80, normal blood sugar fasting less than 100, and cholesterol levels total less than 200.
LDL levels less than 130 and quit smoking these all will reduce your risk of developing heart disease. If your symptoms are mild in nature, discuss them with your primary care physician or advanced practice provider to verify that it may be heart related.
Your provider may order cardiac testing to determine if your symptoms are related to your heart or may refer you directly to a cardiologist like Dr Boon Lim .
Comments
Post a Comment